User-centred approach to automating healthcare conversations
Posted on
Over the last three years I have had the opportunity to work as an AI Research Clinician at Ufonia – an autonomous telemedicine startup company that is harnessing AI to drive automation in patient pathways. This is through Dora, an automated clinical assistant that conducts routine conversations with patients through a telephone call. Dora is an automated telephone voice assistant that can conduct a natural language conversation with patients. Dora is delivered to patients by a regular telephone call. Ufonia’s user goal is that anyone who is able to receive a telemedicine follow up appointment should be able to receive a Dora call that is simple to use, and can take place at their own pace and convenience. For the patient this is not a high-tech solution; it does not require download of an app, the provision of a device, or any training on how to use it. This is particularly important for the relatively more digitally disenfranchised populations that use healthcare services.
As a patient-facing telemedicine company our clinical and product team work seamlessly together to ensure that there is a constant flow of feedback between ourselves and the users be they patients or public. ‘Patient-centred’ is a term that you will hear used frequently within medicine, healthcare and health tech because although there are many stakeholders, ultimately at the core of what we do is the patient and their health. What this means is designing and implementing health care, and in our case technology, in a way that is responsive and respectful to the needs of the user.
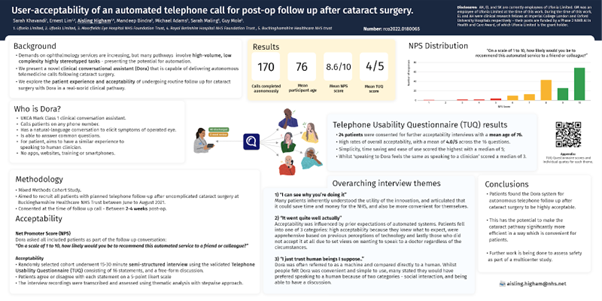
The brilliant thing about Ufonia is that patients have always been at the heart of why we do what we do, and as the company has grown, so has this ethos. In fact our first study was focused on user acceptability, which has been presented and won awards at multiple academic conferences both nationally and internationally. You can read more about it in the EuroTimes.
The importance of Patient and Public Involvement (PPI)
Medicine is an evidence-based discipline and generating the data for evidence through research is a universal principle of healthcare. Research informs policy, policy informs practice and practice impacts the patient. PPI is when patients and members of the public share their views and experiences to help inform activities from designing research all the way through to adoption and implementation of outcomes. This active partnership ensures that the research is being done ‘by’ patients rather than ‘to’ patients. The Oxford Academic Health Science Network (AHSN) and the Patient Experience Research Centre at Imperial College London have excellent definitions, training and resources available.
Ufonia’s approach
Ufonia’s research projects have encompassed patient and public involvement and engagement from the outset led by the brilliant Dr Siân Rees who is the Director of Community Involvement & Workforce Innovation at the Oxford AHSN. Through this we have been able to work with a diverse group of individuals including seldom heard groups and underrepresented communities. As the PPI lead for Ufonia I have observed these focus groups to listen and learn about the experiences patients have had with the current healthcare system, their thoughts on automated telemedicine and reactions to Dora. Dr Rees creates a safe and inclusive environment that enables participants to express themselves openly about their experiences, concerns and the changes they want to see. Formal PPI work amplifies the patient voice throughout product development and implementation. At Ufonia we strive together to ensure that with every iteration patients’ concerns and ideas are built into the product in order to remain as inclusive as possible.
What we’ve gained through PPI
Input from participants is highly valued and has an impact at many levels. Broadly, perspectives from the participants provide nuances to the background of the wider healthcare context and enable us to keep looking at the product through a diverse patient lens. More directly, for example, suggestions from participants with different needs regarding the format of information leaflet about Dora has been fed back to the team. In the cataract pathway, nurses now also use our demo videos in the discharge lounge so patients can hear and familiarise themselves to Dora’s voice for those who need it, alongside the leaflets placed in discharge packs. On a different level, we often find that PPI validates research areas that we are working on. For example, we are developing our multilingual feature as this is an important aspect of our product accessibility. During focus groups multiple participants have raised their concerns that NHS patients speak a diverse range of languages and this can sometimes be a barrier to accessing care. This signals to us that the product road map is on the right trajectory.
It has been fascinating to hear different perspectives and incredibly useful to be able to feed this back to the product team as we ask ourselves: how can we better serve our patient population?
Being part of the DigitalHealth.London Accelerator has meant that we are able to learn from and share our lessons with innovators across the UK who are working on similar challenges in healthtech implementation.
PPI is incredibly rewarding and an important part of our user centred approach. The main take home message is to adopt the user-centred approach early- the sooner you start the more time you have to listen and respond to the patient and public needs.
Get in touch if you want to learn more: sk@ufonia.co
DigitalHealth.London is delighted to publish blogs by the NHS staff and digital health companies we support through our programmes, as well as sector thought-leaders, experts and academics. Any opinions expressed within blogs published on our website are those of the author and not necessarily held by DigitalHealth.London. For more information, or if you would like to write a blog for our website, please email info@digitalHealth.london.
Ufonia is currently one of 21 digital health companies on the DigitalHealth.London Accelerator programme.
The DigitalHealth.London Accelerator is a collaborative programme funded by London’s three Academic Health Science Networks – UCL Partners, Imperial College Health Partners, and the Health Innovation Network, MedCity, CW+ and receives match funding from the European Regional Development Fund.



