Driving digital: Insights and foresights from the health and care ecosystem
Executive summary
DigitalHealth.London connects NHS staff, digital health companies and academics, and equips them to improve the NHS and social care in London through digital technology.
To celebrate our fifth birthday, we started a five-week conversation with NHS and social care staff, industry, patients and academics to hear about their learnings from the last five years and the opportunities for the next five years in digital health.
Insights – The five key lessons from the last five years were:
- Overcoming legacy systems and processes – NHS IT systems and processes need to be an enabler not a barrier to digital health adoption.
- Co-design leads to better outcomes – Involving health and care staff, industry and patients in designing solutions leads to better tools and usage.
- Capacity and capability building is key – Effective NHS change management and digital capacity building is vital to deliver the scale of change needed.
- Digital tools can both increase and decrease inequalities – Digital inclusion for patients is crucial but need not be an excuse for inaction.
- Evaluation is key to adoption – Determining how and what to evaluate in digital health will enable further adoption.
Foresights – The five key opportunities in the next five years are:
- Joining up the system so solutions can scale – Getting the basics right first and connecting systems allows for digital delivery.
- Digital tools offer scope to tackle workforce challenges – There will be a focus on combatting workforce challenges including through utilising AI.
- Digital tools that aid remote patient care have scope to improve outcomes, experience and safety – The remote digital offering must continue to grow to meet the needs of patients to manage their journey though the health system and better self-manage.
- Data saves lives – Data needs to be used to personalise care, predict health issues and to empower the patient to take ownership of their care.
- Go global – Now is the time to go global, both looking for solutions to the challenges of the health and care system, and for our innovators to target global opportunities.
Five years ago, when we established DigitalHealth.London, we set out to make the London the global capital of digital health, building upon our unique innovation ingredients of the NHS and social care, clinicians, academics, technologists, entrepreneurs and investors. Over the last five years digital health ecosystem has now grown and developed more than our expectations, with impressive accomplishments by innovators and the NHS. We are even more optimistic about the next five years, with scope for radical improvement in the way health and care is delivered in the UK, and innovations set for wide-spread adoption and global opportunities.
Thank you to everyone who has contributed to this publication, and we hope that those reading these insights gain as much from it as we did and we look forward to working with you all to realise the potential of digital in health and care.
The DigitalHealth.London team and partners

Introduction
DigitalHealth.London was launched in 2016 by London’s three Academic Health Science Networks (AHSNs) and MedCity, and with additional partnership and funding from CW+ and the Greater London Authority, aimed to create an active digital health market in London through removing some of the challenges that were holding innovators back.
The healthcare landscape was beginning to change, with the creation of NHS Digital, the appointment of NHS England’s first Chief Clinical Information Officer and Chief Information Officer and NHS England announced the selection of NHS Trusts to become funded centres of global digital excellence. The digital health revolution was just beginning and with it came an increasing opportunity for innovation.
There has been a huge cultural change in digital health over the last five years. When DigitalHealth.London began it was difficult to bring the idea of working with start-ups into conversations, whereas now this is more normalised. When we made presentations at health forums five years ago, we were introducing the ideas of digital and the potential benefits whereas there is now an acceptance that innovation is the key to the NHS’s survival, especially in recovering from the Covid-19 pandemic. We of course still face challenges, but the progress that has been made is outstanding.
First came our Accelerator programme, aimed at supporting adoption of high potential digital health companies in London’s NHS and social care, and subsequently the Launchpad programme for earlier-stage companies. We have supported over 120 companies through the Accelerator and a 2020 independent report found that for every £1 spent on the programme through the AHSNs, £12.70 is saved for the NHS. Supporting companies isn’t just beneficial for the NHS, it’s also important for the country’s economy, generating growth and investment. See an example of how the Accelerator has supported a company’s growth here.
DigitalHealth.London has now supported over 120 exciting innovative companies. Not only have they helped tackle the challenges faced by the NHS, but together than have raised over £2 billion of investment into the digital health sector and created over 1400 jobs over the last 5 years.
The Generator programme was developed in 2018 as an expert network to support evidence generation collaborations between academics and digital health companies, to help ensure NHS organisations could feel confident about choosing the right technologies. We quickly realised the importance of developing innovation capability within the NHS as well as helping small businesses, so in 2018 we launched the Digital Pioneer Fellowship programme to support innovators within the NHS to lead and deliver transformation projects on the ground. The programme has supported a total of 97 members of NHS staff across 45 organisations in London and the South East. Our support has not stopped at these distinct programmes, and we have reached wider audiences through running regional accelerators, supporting international collaboration, advising investment firms with identifying good digital health companies and delivering transformation and innovation events for the health sector.
We are proud of what DigitalHealth.London has achieved over the last five years but also of how much we have learnt. Through our many relationships within the ecosystem over the years, we know we are not alone in our learning, with each sector having unique experience and insight to share, as well as distinctive visions for what is important going forward. Therefore, to celebrate our fifth birthday, we started a five-week conversation with NHS and social care staff, industry, patients and academics to hear about their learnings from the last five years and also their thoughts on the next five years in digital health. We asked seven questions across three events to a combined audience of over 300, published 32 polls and questions on social media receiving 718 responses, and published an in-depth survey which was completed by 31 participants. We have summarised the responses here to encourage the spread of these insights, key themes and ideas from across the sector.
DigitalHealth.London has brought together voices from across health and social care – staff, patients and service users, industry and academics – to reflect on learnings from the last five years and the future of healthcare. This publication provides invaluable insights for how we can work together towards the goal of improving people’s care. I would encourage leaders, clinicians and decision makers in health and care to read, share and take action.
Insights – Lessons from the last five years
From improving connectivity of NHS IT systems and connections between healthcare staff and industry, to bringing key stakeholders on the journey and ensuring digital inclusion is brought into the conversation – it is clear that collectively, we have learnt a lot in the last five years about how to better incorporate digital into healthcare delivery.
Digital change is hard! Digital change is still “change” and change in a large organisation has many challenges. Selling the benefits of digital health to the correct stakeholders is key to allow digital health to prosper.
Jack Grodon, Clinical Specialist Physiotherapist at Guy’s and St Thomas’ NHS Foundation Trust
The pandemic has enabled adoption of digital healthcare at pace. What previously took years of change management, stakeholder engagement and adoption of new technology, has been condensed to a matter of months!
Mark Da Rocha, Project consultant and formed Programme Lead at Kent & Medway STP
It is of course impossible to discuss learnings from the last five years without acknowledging the impact of Covid-19. Matthew Gould, CEO of NHSX, said to DigitalHealth.London, “A decade’s worth of digital transformation has happened in the last 18 months. The sense of urgency and compelling need to act has lessened as the pandemic has eased. But the NHS now recognises the need for digital and innovation to be front and centre in health and care vision for the future. If we want the same or better level of care, we need to start doing things differently.”
NHS staff reflected that “necessity drives innovation more so than anything else” and when asked what the best success story in digital health over the last five years has been, many people across our audiences identified that Covid-19, while devastating in so many ways, has also created the environment for some successes. One patient said, “The pandemic has shaken the recalcitrant and the blockers of good care.”
But beyond this there are still many challenges facing our healthcare system and several learnings to act upon. Below are the the five themes, as driven by the ecosystem engagement
Click the + button to expand.
Over-coming legacy systems and processes – NHS IT systems and processes need to be an enabler not a barrier to digital health adoption
One of the most common challenges to digital health innovation identified across all five audiences was challenges with NHS IT systems. Digital health industry participants in particular highlighted legacy systems, limited interoperability and lack of integration with healthcare records as key challenges for implementing new tech. One nurse commented that “connectivity is hard to achieve without standards which in turn are hard to develop and agree across diverse communities.” It was also raised that there is a “poor understanding of interface with social care” and information governance requirements in organisations were identified as a blocker.
Look at the readiness of organisations to adopt innovations, and scale readiness.
Brian Donnelly, Honorary Lecturer in Digital Health, School of Medicine, University of Central Lancashire
Healthcare should lead digital innovation, not digital innovation leading healthcare.
James Gagg, EM consultant, Clinical Director for Urgent & Emergency Care, Somerset Foundation Trust
This was identified not only from an NHS systems perspective but also with digital health innovations often being developed without considering implementation. One individual said they feel there is an “excessive focus on what a digital tool can do over its ability to be implemented in the healthcare system.” One digital health company said, “Too often the tech solutions being presented fall short because of the disconnect between the idea and the practicalities, i.e., it ends up adding to workload, rather than easing it, which impacts uptake.”
The learning I think for any health tech company is to be flexible enough to work with each unique situation as you find it, and at the same time know when to bring standardisation and that accumulated experience to help every NHS organisation.
Jonathan Knight, Co-Founder and CEO at Tefogo
The ability to take risks and test an innovation to show the benefit and impact on health equality was also identified as an enabler to successfully innovate, and it was suggested that there should be “incentives for NHS organisations to take risk.” One participant said that there is “too much variation across NHS organisations with Trusts wanting to find the perfect single solution for them rather than taking the leap and developing with the supplier.”
It is clear that the complexity of navigating systems is real and continues to be an ongoing challenge which is why we created An Innovator’s Guide: Navigating the barriers to digital health, a reference tool for innovators to help navigate the health system and drive progress through digital transformation.
Uday Bose, Country Managing Director and Head of Human Pharma at Boehringer Ingelheim UK & Ireland
For digital health companies, ambiguity and variation of procurement processes across NHS Trusts has been a key pain point over the last five years. Mridula Pore, Co-Founder and Co-CEO of Peppy Health said, “Clear commissioning processes and budgets [are needed]. They are too fragmented and there are too many stakeholders involved. There is also no guarantee of repeated business, which makes it much less attractive to investors.”
Co-design leads to better outcomes – Involving health and care staff, industry and patients in designing solutions leads to better tools and usage.
We need more support on adoption side – but most importantly widening participation in digital design, from the off. So that ‘the next big thing’ in #healthtech reduces and doesn’t exacerbate the digital divide.
Hannah Harniess, Deputy CEO, Care City
Collaboration in design was a key theme of the discussion with several entrepreneurs, saying that co-production of their service/product made the biggest difference for them and that grants that require partnerships with NHS organisations were a great vehicle for this. NHS and social care staff agreed, with one participant saying, “Innovators need to be embedded inside healthcare not sitting outside it.” NHS staff also said that ultimately the biggest enabler for them is engaging the users at the beginning to help shape the direction, particularly if the users are not the clinicians.
Patient and workforce centred disruption to create high quality sustainable healthcare is within reach – strong collaboration between healthcare @DHealthLDN and industry partners will make this possible.
Ian Abbs, CEO, Guy’s and St Thomas’ NHS Foundation Trust
Both the NHS and digital health businesses said that they would previously only get feedback from a working group or select number of wider staff members in the initial stages of design. This led to having to repeat steps and delaying the project when users gave feedback later in the project.
I’m excited about the power of data, what we can do digitally to really drive innovation and research. For me, [it’s about] how we co-create the platforms, tools and space for our brilliant research teams
Lisa Emery, Chief Information Officer at The Royal Marsden and Chair of the London CIO council
Patient centricity has been central to the Digital Pioneer Fellowship programme, sponsored by BI, and has meant that the Fellows are responding to the bespoke needs of the community, to better meet the requirements of society more broadly and to build solutions that truly hold patients at their core. it is critical that any digital health innovation must engage, and ideally co-create with patients from an early stage in the development process to ensure the solution is fit for purpose, so it was great to see the Fellows aligning to these goals.
Uday Bose, Country Managing Director and Head of Human Pharma at Boehringer Ingelheim UK & Ireland
Case study: Creating a GP satnav

Capacity and capability building is key – Effective NHS change management and digital capacity building is vital to deliver the scale of change needed.
It is rarely technology that is the issue in scaling innovation, it is more about the culture, the people and the systems. We tend to focus on the technology and not the people. Constant attention to the messages that the leadership gives to the wider team around technology is key, as well as looking at structures, incentives and also how easy it is for frontline leaders to do the right thing
Matthew Gould, CEO, NHSX
Closely related to co-design is the importance of effective change management. The importance of engaging with NHS staff and stakeholder engagement was apparent throughout the conversations. Louise Booth, Programme Manager for Health Education England said, “Digital is as much about the people as the tech.” There was agreement that this is partly achieved through co-design but the importance of having leaders who recognise value of digital and organisation buy-in at the highest level was seen as crucial. One NHS staff member said, “If the execs don’t live and breathe digital health, innovation fails”.
Our biggest learning, by some margin, is that healthcare is a team sport; it’s all about the people. With a strong ecosystem of people supporting each other, lifting each other up rather than pushing each other down, it’s possible to do amazing things – the response to the pandemic and the adoption of digital over the last two, really tough years prove that.
Thomas Whicher, Founder at DrDoctor
This also has implications for digital capacity building. When asked whether there was a digital literacy gap in the workforce, 83% of 120 participants said yes. Digital health industry participants noted that because bandwidth of staff within the NHS is low, it is therefore vital to give them the support they need to adopt innovations. One participant said that “Doing digital innovation and change badly can frustrate the workforce”, while a Physiotherapist said, “System design is a huge issue. Ever been on a training course to order from Amazon or use an iPad? No. Need a training course to order basic tests at a hospital? Yes, multiple. This affects confidence of workforce and reduces engagement to change.”
Digital and care shouldn’t be opposing forces. Involving clinical staff from the beginning is essential… [There is a] need to professionalise the role of informatics clinicians.
Joe Rouse, Digital Nurse Specialist and Registered Children’s Nurse, Buckinghamshire Healthcare NHS Trust
Case study: Pioneering simulation-based medical teaching

One form this support can take is through partnerships, for example that of DigitalHealth.London and Chelsea and Westminster Hospital, through which DigitalHealth.London provides guidance on working with, and introductions to, digital health companies. James Varley, Finance Director at CW+ (the Trust’s charity), said it is “a fantastic partnership, built on our shared vision to accelerate the adoption of digital health innovation across the NHS. Together, we are implementing innovative initiatives that not only respond to the changing needs of patients and staff in a rapidly evolving digital landscape but are hugely successful in ensuring greater numbers of patients benefit from emerging new technologies faster.”
The DigitalHealth.London Accelerator is a great example of an AHSN initiative supporting economic growth, illustrating how innovators can benefit from local relationships in the NHS, as well as receiving support to scale adoption through collaborative working with AHSNs and their partners.
Professor Gary Ford, Chair of the AHSN Network
Digital tools can both increase and decrease inequalities – Digital inclusion for patients is crucial but need not be an excuse for inaction.
Digital could be a real force helping us to address inequalities, allowing us to reach people and provide services in different and more effective ways. It will be important to ensure that every digital programme is designed with the knowledge of how it will impact different parts of the population, making sure the patient voice is heard, the data sets used to verify and develop algorithms are representative, and that equally good non-digital alternatives are always available.
Matthew Gould, CEO, NHSX
Digital inclusion was a big topic of discussion over the five-week engagement campaign, and it was evident that this has been a significant area of learning over recent years. One participant said, “digital technology can adversely impact communities if we don’t take digital inclusion seriously and plan it in.”
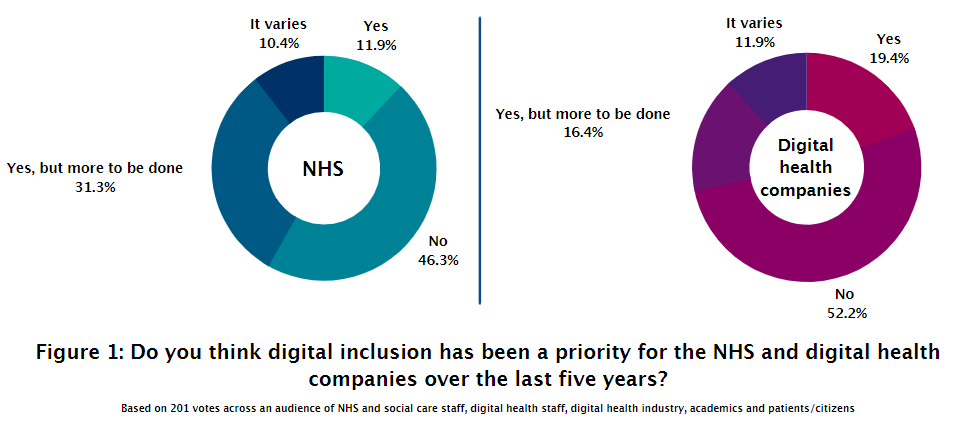
When asked whether digital inclusion had been a priority for the NHS over the last five years (Figure 1), 46.3% of responders said no and 43.2% said yes. 52% said they did not feel it had been a priority for digital health companies. This varied based on the audience, with NHS and social care staff taking a less optimistic view of digital health company prioritisation of digital inclusion.
Whether you’re working in the NHS, whether your in social care, digital education is key for utilising technologies. For any technology we’re deploying, digital education is there to provide the skills and competencies for both the service users and the workforce.
Saira Arif, Customer Success MAanger, ORCHA
Co-design was identified as a key weapon against digital inclusion as well as focusing on “how the pathway enables individuals to achieve the same outcomes irrespective of their level of digital literacy and access” (Oliver Brady, Programme Director – Diabetes. Cardiovascular Disease Prevention, and Mental Health at Health Innovation Network). One patient flagged the importance of acknowledging that digital might not always be the solution and that it may be inappropriate for some situations and settings.
Evaluation is key to adoption – Determining how and what to evaluate in digital health will enable further adoption.
Evidence generation for digital health technologies has been a focus for DigitalHealth.London for some time and the discussion revealed this has been the case across the sector.
Evidence generation for digital health is a very complex area and it is the hyper complexity of healthcare systems which can make it difficult to measure impact. Randomized control trials are often seen as the gold standard but there is also a need for real world case studies to see whether a digital health intervention is going to work in everyday life.
Professor Trish Greenhalgh, Professor of Primary Care Health Sciences, University of Oxford
One NHS/social care participant said their biggest learning over the last five years was “understanding more about the challenges of and approach to evidence generation around digital health technology… a greater understanding of the different perceptions of and need around evidence across different stakeholders (e.g., SMEs, health/care commissioners and providers, and patients/public).” When asked about how to ensure long term sustainability of digital health, one participant said, “by generating evidence that shows effectiveness in the real world and bringing this to the attention of GP’s, CCG’s etc.”
There should be a greater focus on health service research looking at the implementation challenges and workforce issues. I think there is enough funding available to generate evidence of effectiveness.
Mike Wright, Innovation Business Partner, Chelsea and Westminster Hospitals NHS Foundation Trust
On the digital health industry side companies have learnt a lot about the importance of generating evidence but acknowledge the difficulty in knowing what evidence to produce and how. One industry professional said, “Digital health is still treated as if it’s a branch of pharmaceuticals and expected to be assessed in the same way.” while another identified an issue with the requirement for companies to show evidence of in-year savings.
One very important area that we at MedCity are passionate about is equipping companies with the knowledge of how generating good evidence can be a tool to enable adoption and market access.
Neelam Patel, CEO of MedCity
Foresights – Opportunities in the next five years
As we turn towards the future, the focus changes to how digital can help tackle the challenges the NHS and social care is currently facing and is likely to face in the years to come, in line with the priorities set out in the Long Term Plan. Digital was seen as an opportunity both for those longstanding NHS challenges, but also issues around the recovery from the pandemic and matters highlighted by the pandemic like variation across the country and tackling health inequalities.

We asked an audience of NHS staff and SMEs what their organisation’s priorities were for the future. The companies shared that theirs will be fundraising to allow them to enter the next phase of development and forming partnerships with NHS organisations. Priorities for NHS staff included delivering safe care to patients, transitioning away from paper-based systems and working more effectively with data, both making it easy for staff use data it to improve delivery and care.
The demands on the system are likely to intensify before they recede. A great time to innovate.
Anonymous participant
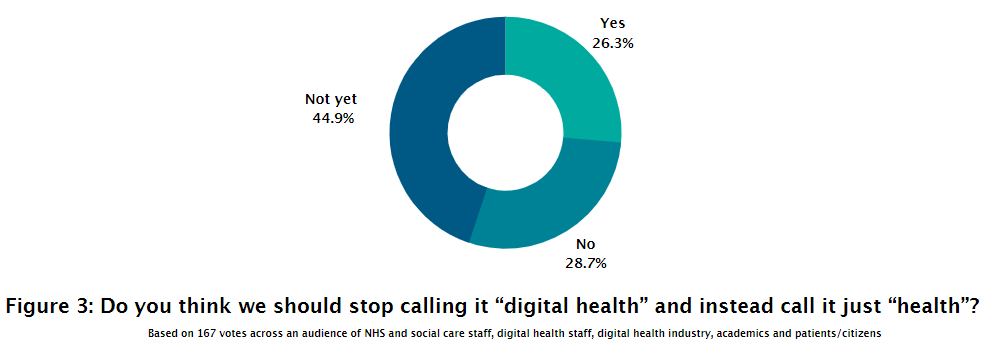
When talking more specifically about the future of digital health, the majority of people felt that we should continue to use the term “digital health” as opposed to simply calling it “health”. Reasons for this included the importance of defining the changes which are being introduced for patients and staff, and the workforce not being ready. One member of NHS staff said, “We need the change makers & digital champions to embed and then digital could be considered BAU in healthcare.” Three patients surveyed felt we couldn’t stop calling it digital health yet because “we still face huge challenges to demonstrate all the benefits of digital transformation and of digital services.” On the other hand, Tom Allen, NHS Lead at Amazon Wed Services (AWS), said he liked the idea that “we stop calling it “digital” health, in the same way we don’t say digital shopping.”
Out of crisis can come opportunity, with the pandemic accelerating the roll-out of digital health services across the NHS. Over the next five years, we need to boost and embed digital innovation that empowers the workforce, allows patients to manage their conditions, and reduces health inequalities.
Suzanne Ali-Hassan, Deputy Director – Commercial and Innovation, UCLPartners
As the discussion around the next five years in digital health continued, five key opportunities emerged.
Click the + button to expand.
Joining up the system so solutions can scale – Getting the basics right first and connecting systems allows for digital delivery.
When discussing the next big thing in digital health, the first common theme was not necessarily about exciting new technologies but was more of a reality check. The first theme was the significance of getting the basics right. Then joining up the systems is needed to deliver the potential from digital delivery of health and care. This included building the infrastructure for digital health innovation, availability of APIs, integration of technologies with the NHS app, local and regional information exchanges and integration.
We need to be very careful to remember to address the basics. It’s easy to jump ahead to exciting innovation but that won’t work unless we have developed the basics with that.
Anonymous NHS/social care staff member
Digital tools offer scope to tackle workforce challenges – There will be a focus on combatting workforce challenges including through utilising AI.
Combatting workforce challenges is one of the main opportunities for digital in the next five years, including equipping of the workforce with new models of working, digital knowledge and tools.
Often when it comes to implementing digital solutions the focus is on the tech itself. But it also vital to think about how we are bringing innovation capability to the workforce and energising the people who are implementing that innovation.
Yinka Makinde, Director of Digital Workforce and Professionalisation, NHSX
This correlated with predictions of training healthcare professionals to use digital tools effectively, as part of their core education. Health Education England is set to launch a self-assessment tool in Spring 2022 for all NHS staff to assess their own digital skills and be directed to relevant e-learning. DigitalHealth.London’s Digital Pioneer Fellowship, which has been shortlisted for the HSJ Workforce Initiative of the Year Award, is an example of a free programme providing training NHS and social care staff to implement digital solutions.
The NHS Graduate Digital, Data, Technology Scheme (DDaT) has been designed for high potential graduates interested in a fast-track career in Digital, Data and Technology. The purpose of the scheme is to develop the NHS Digital, Data and Technology leaders of the future. DDaT trainees have the opportunity to undertake a two-year rotational scheme in roles, which could be as an information governance analyst, data analyst, junior change/project manager, software support analyst, cyber security engineer or junior networker.
AI and machine learning will transform healthcare in the next five years. From helping automate healthcare to supporting with decision making and improving health outcomes – the opportunities and benefits to the workforce are vast.
Elias Zapantis, Deputy Head, Commercial and Innovation, UCLPartners
When discussing efficient use of staff, AI was also highlighted as a key supporter of the workforce. Many believed that Artificial Intelligence (AI) and Robotic Process Automation (RPA) would soon be used to replace repetitive tasks, support clinical decisions and triage patients through chatbots, thereby freeing up staff time for other vital tasks.

Case study: The generation of Mendelian’s evidence portfolio
Digital tools that aid remote patient care have scope to improve outcomes, experience and safety – The remote digital offering must continue to grow to meet the needs of patients to manage their journey though the health system and better self-manage.
Covid-19 accelerated the use of remote monitoring and virtual consultations, and in this discussion, there was general agreeance that use of these tools will continue to grow and evolve to build an even more robust remote offering. Patient survey participants specifically called out telemedicine and mobile diagnostics as their “next big thing” in digital health.
Case study: Digital remote monitoring in care homes

Video consultations are set to become the norm and can complement face-to-face interactions. Participants felt that the focus of the next few years should be “supporting the move of care out of physical/location-based settings.” One participant said, “the cohort of patients with LTCs [Long Term Conditions] and co morbidities is getting younger. Clinicians need to find new ways to support patients who are less able or willing to access care in a face-to-face setting.” while another said, “younger people [are] expecting digital as the first option. There is a need for more convenience with healthcare access.”

Case study: Implementing a non-contact method of monitoring patients
Another participant identified the ability to provide asynchronous patient care as an upcoming trend as “a lot of healthcare activities do not require the healthcare professional and the patient to be available at the same time, let alone the same room.” This included the evolution of remote diagnostics, “integrating real time data from connected devices to patients and clinical teams, detecting problems and providing solutions before there is a serious health problem.” These solutions also offer significant opportunities as part of elective recovery, supporting people to ‘wait well’ before and after a healthcare procedure. Many highlighted that this would likely result in a hybrid form of healthcare delivery going forward.
As innovators and clinicians we need to be cognisant that we have a global climate health emergency going on and any solution that we bring to the NHS needs to be sustainable and reduce the carbon footprint of the NHS.
Katrina Mason, Otorhinolaryngology Resident, St George’s University Hospitals NHS Foundation Trust
A larger remote offering to those who can and want to take it up also has the additional benefit of reducing the number of journeys to and from hospital, thereby reducing the NHS’s carbon footprint and helping it toward its goal of delivering a net zero NHS by 2045. Sir David Sloman, NHS Regional Director for London, stated that “20% of traffic on London’s roads is people going back and forth from A and E.”
Case study: Refining the Feebris value proposition to meet NHS needs

Data saves lives – Data needs to be used to personalise care, predict health issues and to empower the patient to take ownership of their care.
Sharing data during Covid allowed us to adapt services fast and identified that there was opportunity for research and planning.
Rishi Das-Gupta, CEO, Health Innovation Network
The value of data in healthcare delivery was apparent across the conversation. One participant said, “the NHS has been sitting on an overwhelmingly valuable treasure trove of data that needs to be fully exploited – it has been progressing very, very slowly!”
Data can be used to provide personalised medication and to provide “predictive screening of healthcare issues, changing the system to being proactive rather than reactive”. This aligns closely with the potential of increase in remote monitoring of patient data and use of wearables. One participant wanted to see “accessible and linked data for all (patients, HCPs, academics, QIP etc)”.
My own biggest learning in digital health has been the ability to have a patient portal where I can easily access all my results, appointments and letters, and being able to sync this with apple health. It’s also better for the environment, theoretically, as I don’t need to have letters sent through the post.
Liz O’Riordan, Author, Speaker, Broadcaster and person living with Breast Cancer
This value of data to the patient was also a strong theme spanning across our audiences, with the focus on giving patients access to their own medical records. When asked what impact they’d like digital health technology to have on them in the next five years, one patient/citizen said: “Continue to add to the benefits I already get from using a Personal Health Record.” It was suggested that as patients realise that they can own their own health information and use this to advocate for their own healthcare, the more demand there will be for access and the healthcare system needs to be ready for this.

Case study: The evolution of Fibricheck’s NHS knowledge and network
We need culture change and education. All GP systems are capable of giving full record access to the patient ,yet it is not advertised and repeatedly refused despite a mandate in the GMS contract. Input from 2 care is visible and useful and @patientsco @OneLondon4 are making huge progress. This just needs wide[r] adoption.
“Cancer Mum” on Twitter
Data privacy and governance was an issue raised with this but technology solutions such as fingerprint and iris technology were suggested as a safety measure as well as “digital passports / platforms where everything a patient needs is in one place, a personalised marketplace of sorts.” Clear communication to patients of the regulation of information was also recommended.
The ability in which digital health can generate and harness data, information and insights (big data) will ultimately transform peoples’ health and wellbeing. Providing the right information, to the right person and in the right time (whether this is lifestyle changes, managing a current health condition or just navigating / communicating with health care providers) is the means in which we can achieve on-demand, preventive, predicative healthcare and precision medicine.
Nigel Brokenshire, Head of Digital Healthcare UK, Bayer
Case study: Scaling a self-management solution across South West London

Go global – Now is the time to go global, both looking for solutions to the challenges of the health and care system, and for our innovators to target global opportunities.
London is one of the most exciting digital health and care hubs in the world. We are also an international city, and our worldwide connections allow us to bring in expertise from other countries, source innovations from across the globe and, perhaps most importantly, share the fantastic developments we’ve made in the digital health space for the rest of the world to learn from and adopt.
Theo Blackwell MBE, Chief Digital Officer for London
We have seen significant developments around digital health in London and the UK over the last five years, however learning from other countries is also vital to the future of digital health. James Varley, Finance Director at Chelsea and Westminster Health Charity, encouraged the sector to “look to where solutions are successful elsewhere and learn.”
Some of the world’s most exciting digital health work is happening here in the UK. The NHS has a lot of knowledge to share, and there is also much we can learn from other countries. It is vital we use these connections to promote effective ways of improving patient care and work environments for busy NHS staff.
Dr Timothy Ferris, Director of Transformation at NHS England and Improvement
We can learn from other country’s healthcare systems including more flexibility and a willingness to test, better commissioning models and successful transfer of health records. One digital health company shared the thing that has made the biggest difference for them was “Pre-sales trials in California and Texas that we simply wouldn’t be able to do here.”
Speed and agility matters in digital health. We offer structure when it comes to regulation and evidence, but flexibility driven by need is what I see enabling innovation in other parts of the globe.
Hassan Chaudhry, Global Digital Health Specialist, Healthcare UK, Department for International Trade
Better commissioning models! German social health insurance companies are beginning to develop and deploy financial tools for procuring patient facing digital health solutions – we need something like this otherwise it will remain a cottage industry with decision making focusing largely on cost reductions. Currently many digital health solutions are seen as cost pressures to be managed.
Mike Wright, Innovation Business Partner, Chelsea and Westminster Hospitals NHS Foundation Trust
Conclusion
When we asked what DigitalHealth.London and organisations like us should focus our efforts on over the next five years, 41% said long-term sustainability of innovations while 33% said supporting NHS staff. Through supporting the sector to implement these practical recommendations and as part of our Accelerator, Launchpad, Generator and Digital Pioneer Fellowship programmes, we aim to do just that. We will also work with international partners to support shared learning and the global growth of digital health.
Acknowledgements
Thank you to all those who contributed to our fifth birthday conversations and to DigitalHealth.London’s supporters, funders and advisors for your support over the last five years.
We believe that if the sector acts based on the lessons and capitalises on the opportunities shared here, we will see a truly impactful change in the digital health landscape in the next five years.



