Changing winds COVID-19, digital innovation and the frontline NHS
Posted on
“You felt the wind change before you heard the bombers or felt the bombs,” said a patient of mine describing her experience of WWII. “I can feel the wind changing again” she added speaking just days before the COVID-19 lockdown began, almost foreseeing what was to come.
At 91 years old, her words rang true and my life as an NHS consultant was turned upside down, like so many others PPE, long shifts, apprehension, an unpredictable future, and re-affirmation that many things we did in the NHS were simply outdated. Not just the over-reliance on pen and paper, but many NHS processes, workflows and information haven’t caught up with advances in digital technology we have seen in almost every other part of our lives.
As well as being an NHS Consultant and a patient, I am a co-founder of LifeBox a digital health SME. As the Medical Director I lead a team of 7 NHS Consultant Surgeons, Anaesthetists and Radiologists with over 200 years of combined NHS experience. We are united in our recognition of the need to provide better care and support to patients before they have surgery and doing that by aligning clinical expertise with the benefits of digital technology. Just as importantly we understand the need to demonstrate to hospitals how digital process change was not threatening but empowering as staff are supported to best utilise their clinical skills.
A UK First – how LifeBox works for patients
My 91 year old patient, weeks before needing an operation, had already had her health assessment done remotely using the LifeBox app, with her family to support her. It proved a cornerstone to her pre surgical care and education, meaning her visits to hospital were significantly reduced but she felt empowered and understood the surgery she was about to undergo. By using the Secure Virtual Clinic (SVC) function of LifeBox, she was able to have a video consultation with the hospital nurse, take a picture of her prescription sheet and send it digitally to the hospital. The physiotherapist was able to have a virtual tour of her flat to understand discharge mobility issues. Following surgery, she had her discharge exercise videos, medication advice and wound care advice sent to her via the Secure Virtual Clinic portal. She in turn was able to send us pictures of her wound and video of her recovery by simply using her phone. This was revolutionary, it enabled the patient to receive the highest possible level of care in the safest and most effective way and was a UK first. Digital innovation allowed for the best parts of traditional hospital care to be delivered remotely with the benefit that multiple healthcare professionals could interact with the patient seamlessly providing complete virtual care. The combination of the SVC with the pre-operative health assessment (ePOA) is the UK’s first end-to-end digital surgical journey.
35000 UK patients already benefitted from LifeBox’s remote management of the pre-surgical care, in the year before lockdown. In one CQC outstanding hospital, they reduced face-to-face appointments by 70 percent by introducing the LifeBox system. Independent scientific and financial presentations on the successes of LifeBox made me feel proud of what our team had achieved – then the wind changed.
COVID-19 – the wind changed
Elective surgery dwindled overnight as hospitals were inundated with COVID-19 victims. The need for our app to support elective surgery reduced dramatically. Then came a call from two of our London hospitals who became cancer centres for the NHS during COVID-19. Their staff and patients were understandably frightened of face-to-face contact but there was still a need for support and quality care. These hospitals, therefore, reached out to us as they wanted to use the LifeBox app to support their vulnerable and sick cancer patients. It minimised the need for these patients to attend hospital before vital, often life-saving surgery and benefited staff. Anybody who has worn PPE for more than an hour will testify to how unpleasant the experience can be. LifeBox’s simple digital process of remotely assessing and risk stratifying patients, helped to avoid unnecessary face-to-face contact for these cancer centres. We proudly helped over 1000 patients through the app during the initial COVID-19 lockdown period.
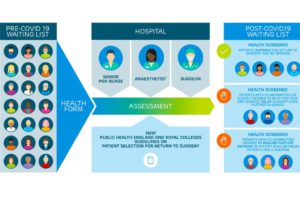
The ability to digitally and remotely assess patients whilst allowing hospitals to dynamically risk stratify health co-morbidities form some of the many unique features of the LifeBox platform and where digital health comes into its own. By filling in a smart electronic pre-operative health assessment, it enables patients to be health assessed for surgery from the comfort and safety of their home, protecting them and the staff from unnecessary hospital visits. All essential members of the patient’s hospital team can have sight of this pre-surgical information so that seamless care can be delivered.
Innovating NHS challenges of today and tomorrow
Born out of the frustration our team of current NHS surgeons and anaesthetists experienced, we knew that the design of the LifeBox platform needed to work within the existing pathways and structure of the NHS. Our ambition was to improve the process around pre-surgery and to do so, we needed to allow remote delivery of health information by patients whilst providing clear concise health information and outcome assessments such as Patient Reported Outcome Measures (PROMs). At the same time hospitals needed a live dashboard with front loaded patient health information on which to make key clinical decisions. Its application has helped all 8 hospitals we are working with, to stratify and organise their backlog of patients in these COVID-19 times. Our ninth hospital has just gone live and our 10th is due to go live next week.
Now, as the acute effects of COVID-19 lessen in the NHS, our strength to help hospitals return to surgery has really come to the fore. With NHS England Referral To Treatment (RTT) waiting times show over 26,000 patients waiting over 52 weeks for an operation and a total of 3.3 million patients in the March 2020 figures, the pre COVID-19 NHS challenge is now even greater. It is clear that the traditional model of hospital-based peri-operative care with onsite face-to-face pre-operative consultations, in a one size fits all approach, is no longer suitable. Now we have mature, tested digital solutions available and rapidly implemented with the associated process changes, we cannot simply go back to the business as usual of lengthy face-to-face appointments.
By triaging thousands of patients using LifeBox, waiting lists can be tackled remotely, operating lists carefully populated, cancellations minimised, and recovery and discharge optimised- all by accurate, digital, clinically driven acquisition and communication of the patients’ health status.
We were delighted to have successfully gained a place on the DigitalHealth.London Accelerator programme in 2019. We have greatly benefitted not only from their knowledge of the health landscape in London and beyond, but the support and education on the complexities of business management. This has helped us as clinicians communicate and translate our clinical solution to those busy hospitals and staff who can benefit the most. Now the future looks promising and busy as LifeBox is seen and accepted as a careful integration of the quality of hospital care which is supported by digital technology to take the NHS care for the patients forward through COVID-19 and into the future


